Treating Schizophrenia
- The goal of schizophrenia treatment is to reduce the frequency and severity of psychotic episodes, as well as to improve the functional capacity and quality of life of individuals with schizophrenia, ultimately resulting in patient recovery and reintegration.
- Therapeutic guidelines promote early intervention since a shorter duration of untreated psychosis is associated with better prognosis.
- Pharmacotherapy for schizophrenia usually involves monotherapy with antipsychotics; second-generation antipsychotics are often the first line of defense in a multimodal treatment strategy, although poor adherence is common and often leads to relapse.
- Non-pharmacological treatments involve interventions including psychotherapy, occupational therapy, social skill training, and exercise.
In this section
What’s The Goal?
The goals of schizophrenia treatment differ according to the phase of illness. Early intervention is a key to more a favorable prognosis for patients since the duration of untreated psychosis is associated with worst treatment response, poor symptom control, and worse overall functional outcome for patients with schizophrenia1.
In the acute phase of illness, treatment is aimed at preventing harm, controlling disturbed behavior, reducing the severity of psychosis and other symptoms (eg, agitation, aggression, negative symptoms, affective symptoms), and bringing about a return to the best level of functioning2.
During the stabilization phase, a successful treatment regimen is continued for at least 6 months to minimize the likelihood of symptom recurrence or relapse. When a patient is stable, antipsychotic medications substantially reduce the risk of relapse and their continued use is strongly recommended to ensure that symptom control and remission are sustained and the level of functioning and quality of life are adequate or improving2. Throughout treatment, it is critical to assess adverse effects and adjust pharmacotherapy to minimize treatment-related issues.
Long-term treatment goals for patients with schizophrenia include improved management of negative symptoms, full control over poorly managed positive symptoms, and enhanced patient function and quality of life3–5.
Remission and recovery are the ultimate goals for patients with schizophrenia, although these concepts may mean different things in different stages of the disease. Remission of psychotic symptoms within the first year of treatment occurs in 70%-80% of individuals6 and remains stable with ongoing comprehensive treatment7. However, there is a high percentage of relapse (80%) that is largely attributable to discontinuation of antipsychotic medication rather than to the effects of the disease process8,9. Recovery, which is defined as sustained symptom remission with social and vocational improvement is realized by 15% of patients10.
The Goal of Schizophrenia Treatment11
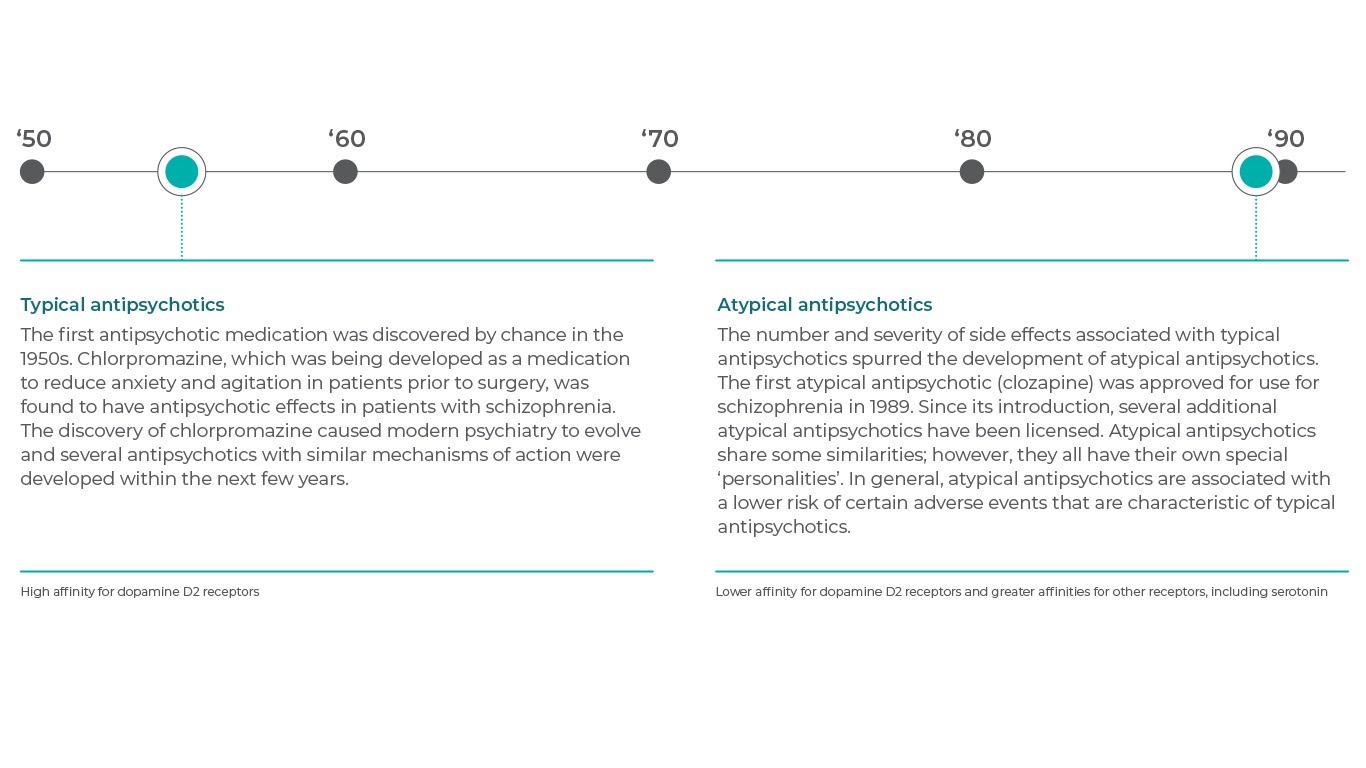
First-and Second Generation Antipsychotics
…It’s All About the Mechanism of Action
Antipsychotic medications have been the foundation of treatment in schizophrenia since the discovery of chlorpromazine over 60 years ago.
All antipsychotics act to block dopamine pathway receptors12. The early agents, which are classified as first-generation (or typical) antipsychotics, all predominantly act by blocking dopamine D2 receptors. Studies have demonstrated that antipsychotic effects are associated with striatal D2 receptor occupancy of 65%–70%, while D2 occupancy greater than 80% significantly increases the risk of extrapyramidal symptoms. Later agents, which are classified as second-generation (or atypical) antipsychotics, have diverse pharmacology, but most have lower affinity for dopamine D2 and higher affinity for other neuroreceptors, (particularly serotonin [5-HT] 2A)than the first-generation agents have13,14. Other sites of action for the second-generation agents include dopamine receptors other than D2 (D1,D3,D4), serotonin receptors (5-HT1A, 5-HT2C, 5-HT6,5-HT7), and muscarinic, cholinergic, and histamine receptors.
Do They Work?
Antipsychotics are more effective than placebo in treating total psychopathology in schizophrenia15. Although the first-generation agents vary in potency and pharmacological properties, they are similarly effective in treating positive symptoms and preventing their recurrence13. Nevertheless, due to severe side effects, they are not the first choice in the treatment of schizophrenia any more. Second-generation antipsychotics are the agents of choice2. They are at least as effective as first-generation agents, although superior efficacy versus typicals is debated14,16. In one meta-analysis, only 4 of the 9 atypical antipsychotics that were evaluated were better than the typical agents in overall efficacy; the others were not more efficacious, not even on negative symptoms17. Other meta-analyses18–20 and effectiveness studies21,22 have also found no clear evidence that atypical antipsychotics were more effective than typical agents in treating overall schizophrenia psychopathology.
Increasingly, atypical antipsychotic drugs with more diverse mechanisms of action are being used for the treatment of schizophrenia in recognition of some efficacy (eg, negative, cognitive, and mood symptoms) and side effect advantages, as well as an appreciation that D2 receptor stimulation is not the only means to treat psychosis.
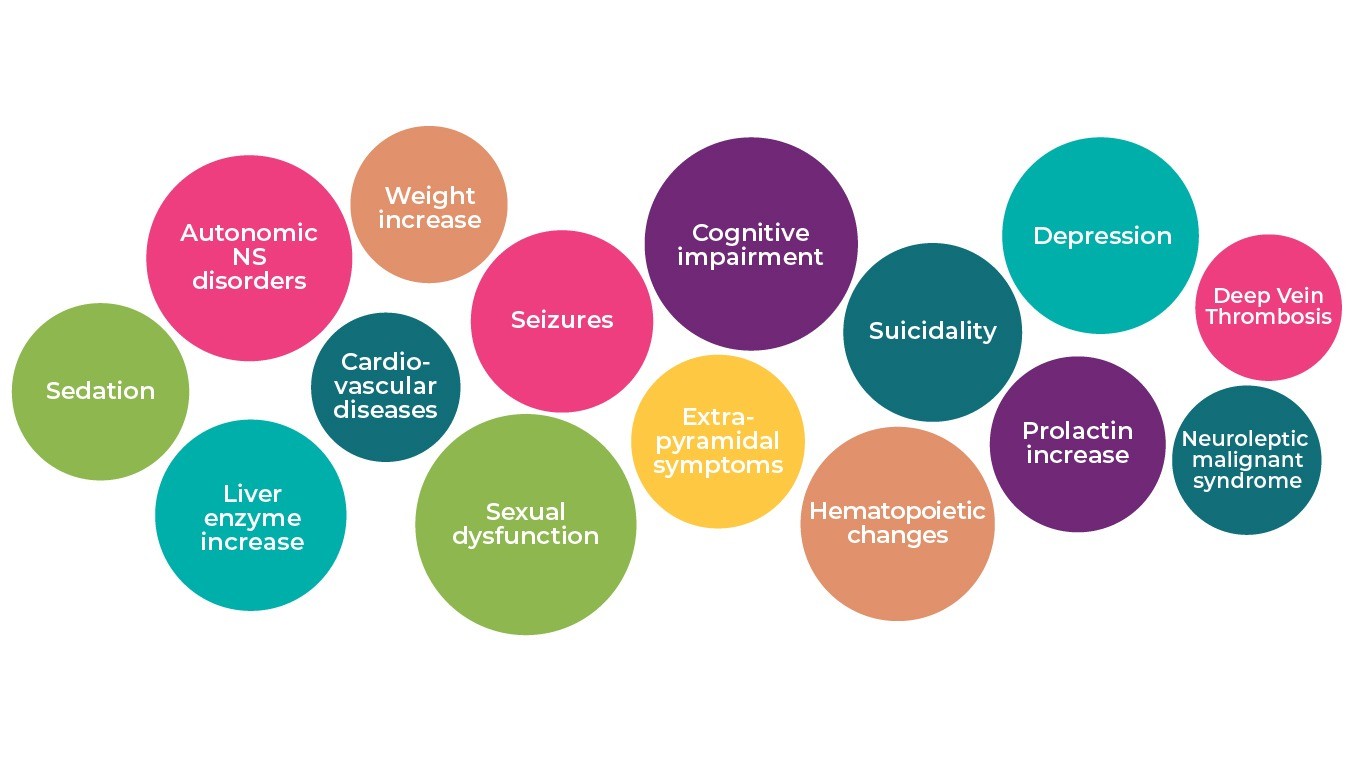
Are They Safe and Tolerable?
There are a number of safety and tolerability issues associated with existing treatments23. The most frequently reported or observed antipsychotic side effects identified in a meta-analysis were sexual dysfunction, metabolic problems, and weight gain, with a longer duration of treatment associated with more severe long-term side effects such as diabetes and metabolic syndrome24.
All of the first generation antipsychotics can produce extrapyramidal symptoms at therapeutic doses, including parkinsonism, dystonia, akathisia and tardive dyskinesia, and increase serum prolactin concentration in the usual clinical dose range13. Although the second-generation agents as a class have lower incidences of extrapyramidal symptoms and tardive dyskinesia than the first generation agents, individual second-generation agents are associated with a greater likelihood of other adverse events that were less of an issue with the first generation agents. Issues such as increased risk of weight gain, diabetes mellitus, prolonged QTc interval, and possible secondary cardiovascular complications are more likely with some second-generation agents13,24.
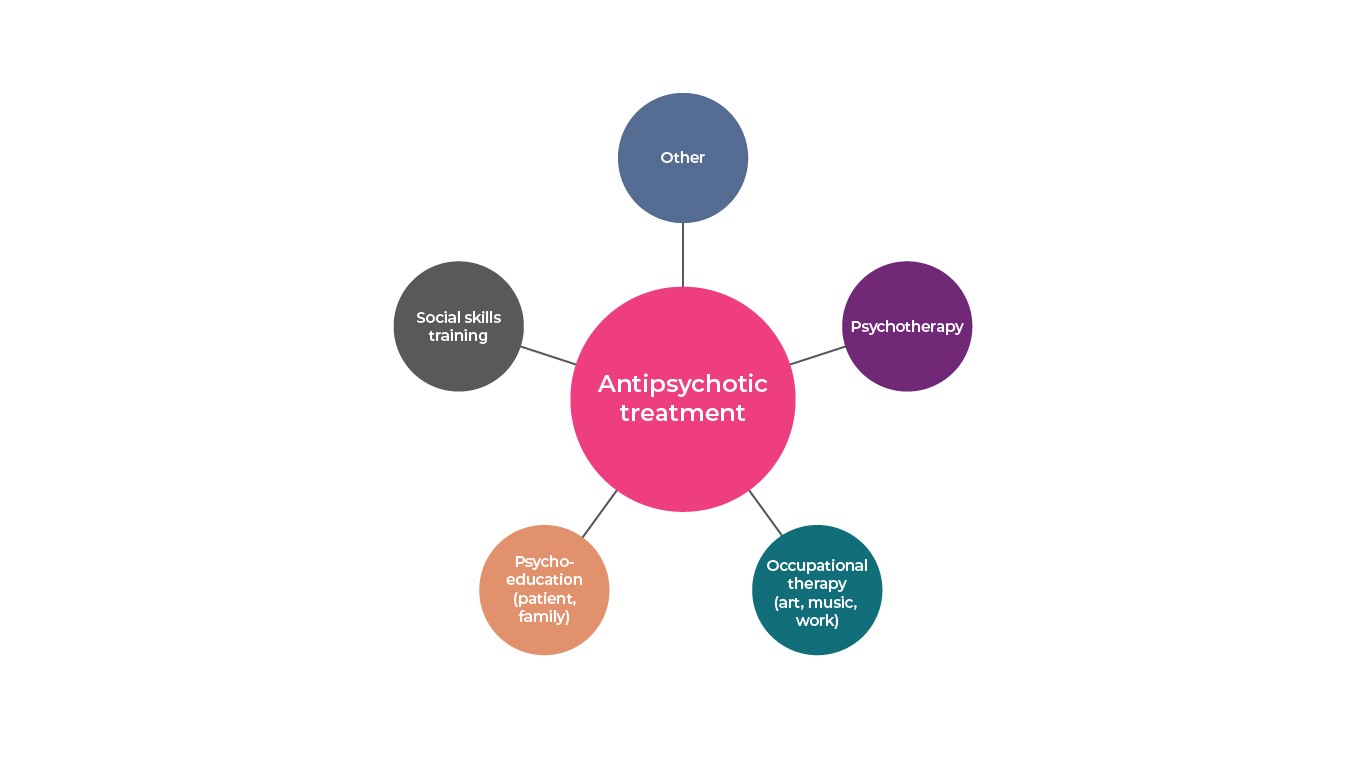
What Else Is Working?
Psychosocial treatments can help improve functioning, including self-care, independent living skills, quality of social relationships, and the capacity to work or go to school. Although treatment of schizophrenia requires pharmacotherapy to be maximally effective, various psychosocial therapies are useful adjuncts to drug treatment13. Psychosocial interventions in schizophrenia target specific domains including core psychopathology (eg, symptoms, cognitive impairment), psychosocial functioning (eg, role functioning, social relationships, self-care), and comorbid conditions (eg, substance abuse, posttraumatic stress disorder, physical health conditions)25.
Schizophrenia multimodal treatment strategy11
Recommended non-pharmacologic practices comprise assertive community treatment, supported employment, cognitive behavioral therapy, family-based services, token economy, skills training, psychosocial interventions for alcohol and substance use disorders, and psychosocial interventions for weight management26. Additional areas of interest for intervention that do not currently meet the criteria for an evidence-based practice include cognitive adaptive therapy, first-episode psychosis intervention, interventions targeting older individuals, peer support services, physical disease management, prodromal stage intervention, social cognition training, supported education, and supported housing25,26. Some of these interventions are specifically tailored to patient age or stage of illness and may prove to be particularly helpful to patients across the course of the disorder.
There Are Limits to Success…
Although antipsychotics are the bedrock of treatment for patients with schizophrenia, not all agents effectively treat all patients with schizophrenia or all symptoms of schizophrenia. For example, approximately 20% to 30% of patients do not respond to antipsychotic therapy. Additionally, 40% of patients have prominent negative symptoms and 80% of patients have clinically relevant cognitive impairment that are generally not responsive to treatment. This suggests that schizophrenia is associated with significant unmet medical needs, functional impairments, and a high burden of illness despite treatment with antipsychotics13,27,28. Lack of compliance with medications is one of major roadblocks to treatment success in schizophrenia. Non-adherence is common, with consequences including inadequate symptom control, relapse, hospitalization, and increased health care resource utilization and cost29. Patients who discontinue antipsychotics may be 2- to 5-times more likely to relapse than other patients8,30,31. Although the reasons for non-adherence to medication are complex (eg, patient attitudes towards drugs and illness, adverse effects, caregiver involvement32, lack of insight in to their illness)33, the inability to remain on medication greatly jeopardizes the opportunity for remission and improved functioning in patients with schizophrenia.
Compliance of schizophrenia patients34
Reference: Adapted from Llorca, P. M. Partial compliance in schizophrenia and the impact on patient outcomes. Psychiatry Res. 161, 235–247 (2008)34
References
- Murru, A. & Carpiniello, B. Duration of untreated illness as a key to early intervention in schizophrenia: A review. Neurosci. Lett. 669, 59–67 (2018).
- Work Group on Schizophrenia. Practice Guideline for the Treatment of Patients with Schizophrenia, Second Edition. Am. J. Psychiatry (2010).
- Kane, J. Commentary: Consensus statement on negative symptoms. Schizophr. Bull. 32, 214–219 (2006).
- Kirkpatrick, B., Fenton, W. S., Carpenter, W. T. & Marder, S. R. The NIMH-MATRICS consensus statement on negative symptoms. Schizophr. Bull. 32, 214–219 (2006).
- Bobes, J., Arango, C., Garcia-Garcia, M. & Rejas, J. Prevalence of negative symptoms in outpatients with schizophrenia spectrum disorders treated with antipsychotics in routine clinical practice: Findings from the CLAMORS study. J. Clin. Psychiatry 71, 280–286 (2010).
- Lieberman, J. et al. Time Course and Biologic Correlates of Treatment Response in First-Episode Schizophrenia. Arch. Gen. Psychiatry 50, 369–376 (1993).
- Girgis, R. R. et al. Clozapine v. chlorpromazine in treatment-naive, first-episode schizophrenia: 9-Year outcomes of a randomised clinical trial. Br. J. Psychiatry 199, 281–288 (2011).
- Robinson, D. et al. Predictors of relapse following response from a first episode of schizophrenia or schizoaffective disorder. Arch. Gen. Psychiatry 56, 241–247 (1999).
- Zipursky, R. B. Why are the outcomes in patients with schizophrenia so poor? J. Clin. Psychiatry 75, 20–24 (2014).
- Jääskeläinen, E. et al. A systematic review and meta-analysis of recovery in schizophrenia. Schizophr. Bull. 39, 1296–1306 (2013).
- Haller, C. S., Padmanabhan, J. L., Lizano, P., Torous, J. & Keshavan, M. Recent advances in understanding schizophrenia. F1000Prime Rep. 6, 1–11 (2014).
- Kahn, R. S. et al. Schizophrenia. Nat. Rev. Dis. Prim. 1, 1–23 (2015).
- Miyamoto, S., Duncan, G. E., Marx, C. E. & Lieberman, J. A. Treatments for schizophrenia: A critical review of pharmacology and mechanisms of action of antipsychotic drugs. Mol. Psychiatry 10, 79–104 (2005).
- Meltzer, H. Y. New Trends in the Treatment of Schizophrenia. CNS Neurol. Disord. – Drug Targets 16, 900–906 (2017).
- Leucht, S. et al. Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: A systematic review and meta-analysis. Lancet 379, 2063–2071 (2012).
- Agid, O., Kapur, S. & Remington, G. Emerging drugs for schizophrenia. Opin Emerg Drugs 13, 479–495 (2008).
- Leucht, S. et al. Second-generation versus first-generation antipsychotic drugs for schizophrenia: a meta-analysis. Lancet 373, 31–41 (2009).
- Geddes, J., Freemantle, N., Harrison, P. & Bebbington, P. Atypical antipsychotics in the treatment of schizophrenia: Systematic overview and meta-regression analysis. Br. Med. J. 321, 1371–1376 (2000).
- Zhang, J. P. et al. Efficacy and safety of individual second-generation vs. first-generation antipsychotics in first-episode psychosis: A systematic review and meta-analysis. Int. J. Neuropsychopharmacol. 16, 1205–1218 (2013).
- Davis, J. M., Chen, N. & Glick, I. D. A meta-analysis of the efficacy of second-generation antipsychotics. Arch. Gen. Psychiatry 60, 553–564 (2003).
- Lieberman, J. A. et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N. Engl. J. Med. 353, 1209–1223 (2005).
- Jones, P. B. et al. Randomized controlled trial of the effect on quality of life of second- vs first-generation antipsychotic drugs in schizophrenia: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS 1). Arch. Gen. Psychiatry 3, 1079–1087 (2006).
- Mohr, W. K. Psychiatric-Mental Health Nursing: Evidenced Based Concepts, Skills, and Practices. (Wolters Kluwer Health/Lippincott Williams & Wilkins, 2009).
- Young, S. L., Taylor, M. & Lawrie, S. M. ‘first do no harm.’ A systematic review of the prevalence and management of antipsychotic adverse effects. J. Psychopharmacol. 29, 353–362 (2015).
- Mueser, K. T., Deavers, F., Penn, D. L. & Casssisi, J. E. Psychosocial treatments for schizophrenia. Annu. Rev. Clin. Psychol. 9, 465–497 (2013).
- Dixon, L. B. et al. The 2009 schizophrenia PORT psychosocial treatment recommendations and summary statements. Schizophr. Bull. 36, 48–70 (2010).
- Ackenheil, M. & Weber, K. Differing response to antipsychotic therapy in schizophrenia: Pharmacogenomic aspects. Dialogues Clin. Neurosci. 6, 71–77 (2004).
- Carbon, M. & Correll, C. U. Thinking and acting beyond the positive: The role of the cognitive and negative symptoms in schizophrenia. CNS Spectr. 19, 38–52 (2014).
- Lindenmayer, J. P. et al. Medication nonadherence and treatment outcome in patients with schizophrenia or schizoaffective disorder with suboptimal prior response. J. Clin. Psychiatry 70, 990–996 (2009).
- Davis, J. M. et al. Dose response of prophylactic antipsychotics. J. Clin. Psychiatry 54, 24–30 (1993).
- Fenton, W. S., Blyler, C. R. & Heinssen, R. K. Determinants of medication compliance in schizophrenia: Empirical and clinical findings. Schizophr. Bull. 23, 637–651 (1997).
- Pompili, M. et al. Unmet Needs in Schizophrenia. CNS Neurol. Disord. – Drug Targets 16, 870–884 (2017).
- Dam, J. Insight in schizophrenia: A review. Nord J Psychiatry 60, 114–120 (2006).
- Llorca, P. M. Partial compliance in schizophrenia and the impact on patient outcomes. Psychiatry Res. 161, 235–247 (2008).
F1000 Prime Reports
Recent advances in understanding schizophrenia.

The problem of therapy success stands and falls with compliance. However only 1/3 of patients are compliant with therapy.
Download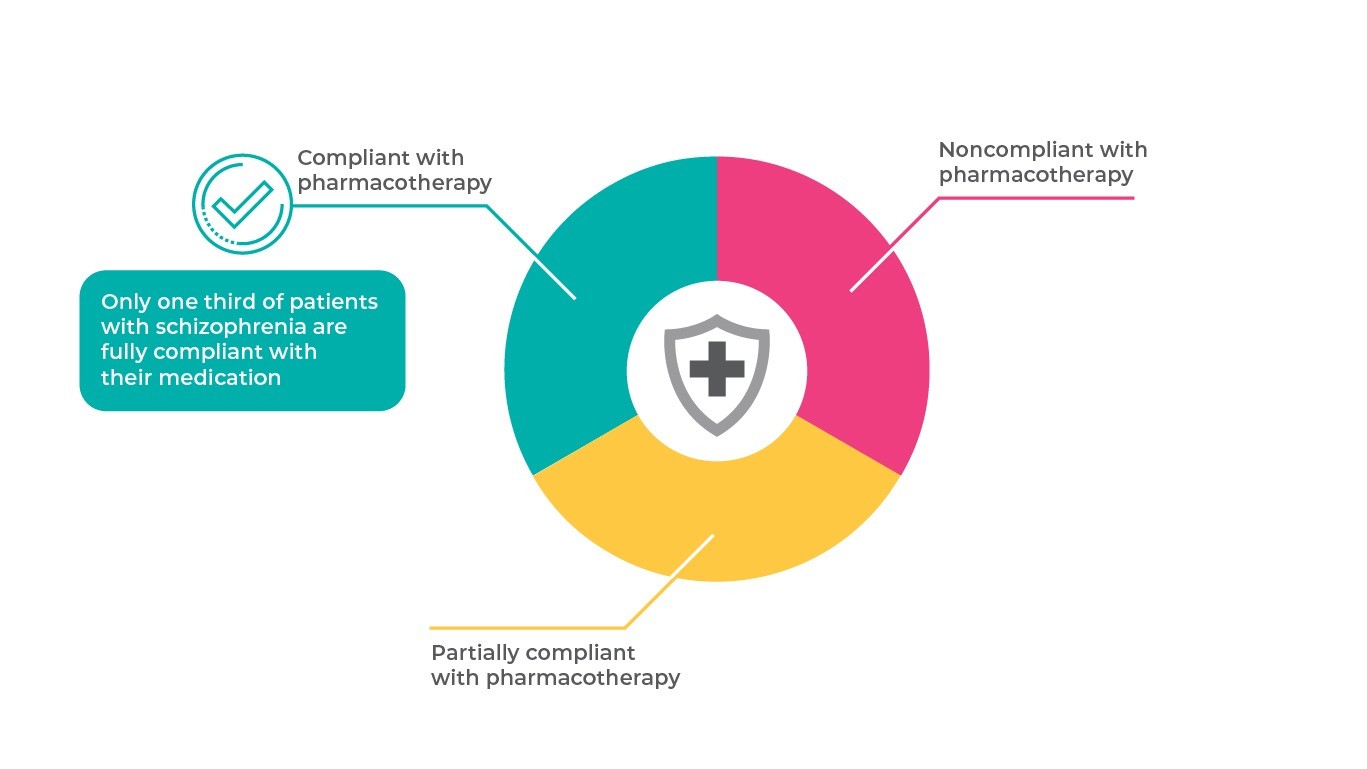
TREATMENT OF NEGATIVE SYMPTOMS
Understanding the relationship between a symptom from a specific domain in schizophrenia and clinical outcomes is important because interventions that just focu
more…OUR PRODUCT’S BENEFITS IN THE LONG …
Atypical antipsychotics need to be effective across the span of illness in patients with schizophrenia. When patients experience acute exacerbation of psychotic
more…