
1.1 How are schizophrenia
and substance use disorders
connected?
It is widely recognized that people living with mental illnesses often face substance use disorders, and the reverse relationship is equally true.

1.1 How are schizophrenia
and substance use disorders
connected?
It is widely recognized that people living with mental illnesses often face substance use disorders, and the reverse relationship is equally true.
‟Dual Disorder‟, the acknowledged medical term
Understanding the interrelation between schizophrenia and substance use disorders has long been a challenge for the medical community. The complexity of the comorbidity often leads to different opinions among experts. Using different and sometimes confusing terms makes things more complicated, especially when trying to diagnose and treat these disorders together.
The lack of a unified term contributes to more confusion and increased. This also leads to what’s called “wrong door syndrome”, where people struggle to find appropriate care for both their mental health and addiction issues. To address this, the World Association on Dual Disorders (WADD) recommends using the term “Dual Disorder”. This term could make it easier for everyone to understand and talk about these conditions in a more consistent and less stigmatizing way.
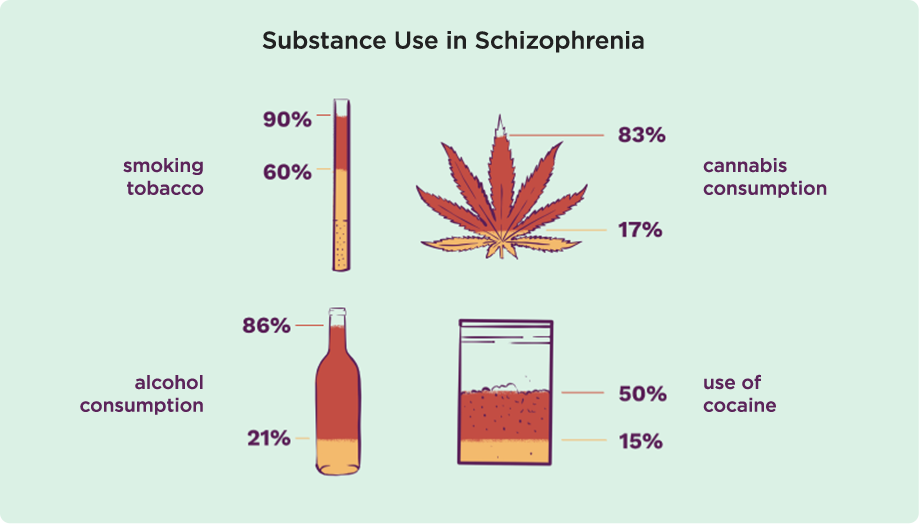
Substance Use in Schizophrenia
Concerning certain substance use disorders, individuals suffering from schizophrenia often struggle with using tobacco, cannabis, alcohol, and cocaine.
The lifetime prevalence rates for these substances range between 60 and 90% for smoking tobacco, 17 to 83% for cannabis consumption, 21 to 86% for alcohol consumption, and 15 to 50% for the use of cocaine. These are more than triple compared to the rates of those in the general population.
Could a psychotic episode trigger the start of substance use?
Experiencing a psychotic episode, particularly the first one, and the manifestation of symptoms (for example, auditory/visual hallucinations, disorganised speech/thinking) can be without a doubt perceived by individuals as STRESSFUL AND UNSETTLING STATE.
Especially when services like emergency or police arrive, the situation may bring about shock.
Being devastating both emotionally and psychologically, such events may lead to compulsive decisions to try or use substances.
Are people with SUD more vulnerable to developing psychotic disorders?
People with psychotic disorders, including those experiencing their first psychotic episode, are more likely to have substance use disorders compared to the general population.
Research shows that substance use is common among individuals with first-episode psychosis, with rates between 30% and 70%.
Compared to healthy individuals, they are more likely to use cannabis daily and to have been smoking it for over five years. Additionally, people with schizophrenia are more often found to have smoked tobacco before the onset of the condition than those without the disorder.
Many researchers also suggest that cannabis use may contribute to an increased risk of developing schizophrenia.
At what point in life are these two disorders most likely to intersect?
Despite drug use and addiction being able to occur at any point during one’s life, it is common for drug use to start in adolescence, the period in which the initial signs of mental illness are most likely to appear.
Co-occurrence of schizophrenia and substance use disorders is also observed in young individuals. About 64 to 88% of adolescents have at least one co-existing mental disorder on top of a substance use disorder.
Young men may be particularly sensitive to how cannabis influences schizophrenia. It is suggested that by preventing cannabis use disorder (CUD), about 1 IN 5 CASES of schizophrenia among young men COULD POTENTIALLY BE AVOIDED. This highlights the importance of spotting and addressing CUD early on, as well as making informed decisions about cannabis policies and access, especially for individuals aged 16 to 25.
While transitioning to young adulthood, (18-25 years), those with dual disorder require support in navigating situations likely to induce changes in different areas that can bring stress, such as interpersonal relationships, work and/or education.