1.2 Why do schizophrenia and substance use disorders overlap?
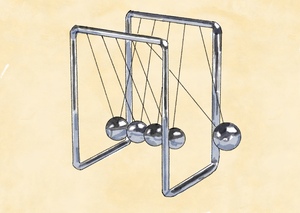
Addiction and mental disorders like schizophrenia often occur together, and this overlap is unlikely due to random factors or measurement errors. This suggests a strong connection between the two conditions.
Discoveries in neuroscience and precision psychiatry are helping us understand how these two disorders develop together. The factors that make people more likely to develop psychiatric disorders are usually present from a young age, even if the symptoms don’t show up until later in childhood, teenage years, or adulthood.

 Genetic Susceptibility
Genetic Susceptibility Neurobiological Imbalances
Neurobiological Imbalances Early Substance Exposure
Early Substance Exposure Self-Medication
Self-Medication Socioeconomic Challenges
Socioeconomic Challenges Stigma and Exclusion
Stigma and Exclusion Substance Accessibility
Substance Accessibility